Robust Theme
Dec 09, 2019 2020-04-08 7:40Robust Theme
Bisphosphonates and the Dental Provider
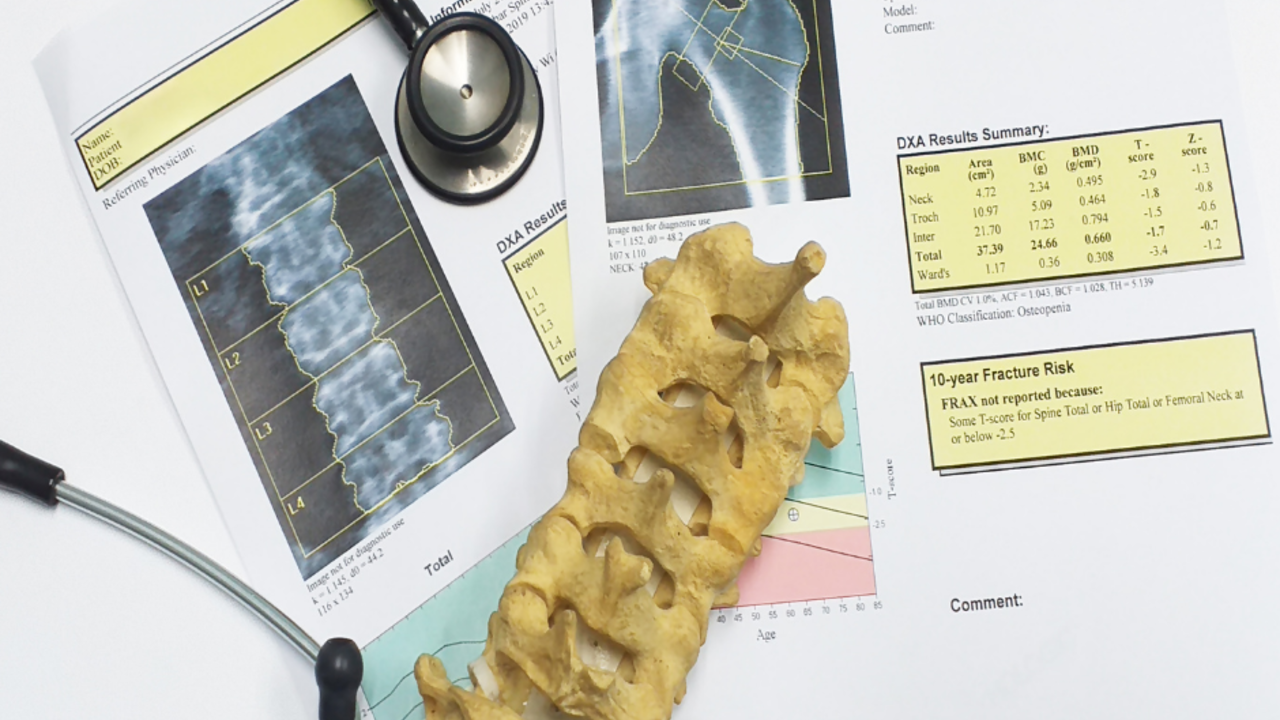
Osteointegration depends on bone formation adjacent to the implant surface and success rates are highest in dense bone and lowest in poor quality, loose trabecular bone. There can be longer healing times or osseointegration that occur in patients with osteoporosis. Approximately three-quarter of postmenopausal women and men over 50 lose post cranial bone through bone demineralization at the rate of 1% to 2% per year and the remaining one-quarter as much as 5% to 8% per year throughout their later life so the chance of implant failure increase in the same rate.1,2,3
Osteoporosis is a skeletal condition characterized by decreased mineral density. Patients who are older with small body size are more susceptible and so are people that have a family history. Additional risk factors are lack of exercise, anorexia nervosa, low sexual hormones, excessive alcohol, and smoking. Osteoporosis can impair the patient’s ability to achieve and maintain implant osseointegration. Primary osteoporosis can be included in either, postmenopausal, age-related changes or idiopathic causes.4 Secondary osteoporosis refers to osteoporosis caused by certain medial conditions or medications that can cause bone loss, increase fracture risk, direct or indirect affect bone remodeling or interference with the attainment of peak bone mass in younger individuals. Treatment of secondary osteoporosis is much more complex than primary. Osteoporosis induced by medications may include glucocorticoids, selective serotonin reuptake inhibitors, aromatase inhibitors, androgen deprivation therapy, certain anticonvulsants, anti-coagulants, hormone deprivation therapy, proton pump inhibitors, thyroid, sedatives and thiazolidinediones.
The treatment of osteoporosis:
According to a 2009 study in the American Journal of Health-System Pharmacists it was estimated that 4.7 million people take oral bisphosphonates. As dental providers we see hundreds of patients annually that take oral bisphosphonates for osteopenia and osteoporosis. Primarily they are prescribed to Caucasian women of slight build but men do take the medications. Other reasons to take bisphosphonates are:
- Multiple Myeloma
- Osteolytic lesions associated with metastatic bone disease
- Hypercalcemia associated with malignancy
- The treatment of Paget’s disease of the bone
IV bisphosphates are sometimes used for patients as opposed to oral bisphosphonates. They were developed to be less irritating and more reliable than oral bisphosphonates. Heartburn and reflux are not an issue because they completely avoid the esophagus and stomach. The dosage for IV use is higher. For example, IV Boniva is given every 3 months and is 3 times as much as the oral Boniva dose. Reclast is given once a year and is 12 times as much as a monthly dose. Using IV bisphosphonates are indicated for cancer patients as well. When used for the treatment of cancer it has been associated with osteonecrosis of the jaw with the mandible twice as frequently affected as the maxilla and there seems to be a correlation between the duration of a patient’s exposure to bisphosphonates and development of bisphosphonate related osteonecrosis of the jaw (BRONJ).
Osteonecrosis, or death of the jawbone (ONJ) dates back to the 19th century where it was called “phossy jaw”. It was an occupational hazard of those who worked with white phosphorus. This was originally found in workers from the matchstick industry in the 19th and early 20th century. ONJ has been reported in patients with cancer who are receiving treatment including bisphosphonates, chemotherapy, and/or corticosteroids.
Clinically ONJ is diagnosed as an area of exposed bone in the mandible, maxilla or palate that typically heals poorly or doesn’t heal over a period of 6 to 8 weeks. The lesion can be painful, but not always however infection is often present. Predisposing factors are dental diseases, dental surgery, oral trauma, periodontitis and poor dental hygiene. All can be factors with an implant candidate. The risk factors for developing ONJ are trauma, female gender, advanced age, edentulous regions, radiation therapy, chemotherapy, steroid therapy, anemia, alcohol or tobacco use, blood dyscrasias/metastatic disease, coagulopathy, prior infection, and surgical dental procedures.6-9 ONJ in connection with bisphosphonates was first reported in 200310, 5-10 years after they uses was approved in the United States for their current indications. Most of the reported cases (95%) have been associated with zoledronic acid or Pamidronate given intravenously to control metastatic bone disease, Myeloma and breast cancer-far most common cancers associated with IV bisphosphonates use and ONJ. 11,12,13 Bisphosphates used in cancer therapy cause great concern about risk of BRONJ. Generally, the risk of BRONJ is 1 in 100,000 but may increase to 1 in 300 after an oral surgical procedure. The majority of BRONJ occur in patients using them intravenously and have co-factors such as smoking, steroid use, anemia, diabetes and immune deficiency.
However, a study released in 2019 that analyzed data from 3,591 postmenopausal women. 1,621 (45.1%) reported they had at least one invasive oral procedure. ONJ was rare with only 5.2 cases for every 10000 patient-years. It was not only rare, but the 11 cases where the outcome was known have healed. Osteonecrosis has been linked more to poor fitting dentures than implants.14 It is prudent to still assess each patient critically before choosing a treatment plan.
Prevention and Management of bisphosphonate associated ONJ:
Before patients initiate bisphosphonate therapy, all medical and dental practitioners should work together and follow a few guidelines.
- All patients should undergo a dental exam to rule out any source of infection
- All medical practitioners should perform a baseline exam
- Invasive dental or/and surgical procedures should be completed before initializing therapy.
- Practice preventive dentistry, oral prophylaxis, dental restorations, and endodontic therapy, and check dentures for irritating areas.
- Schedule routine follow-up every 3 months to check for signs of developing ONJ
- The risks associated with oral surgical procedures such as dental implants, extractions, and extensive periodontal surgeries must be discussed with the patient and weighted against the benefits.
The following recommendations are made by the American Association of Oral and Maxillofacial Surgeons for management of patients on BP therapy and patients with proven ONJ.15
Be cautious. Guidelines for treatment of dental patients receiving intravenous bisphosphonate treatments should be different than for patients taking the oral formulations of these medications. In some studies, oral bisphosphonate therapy did not appear to significantly affect implant success. Minimally invasive implantologists create an environment for success and being aware of all variables ensures that success.
List of Bisphosphonates Brand and Generic
Didronel (Pro) /etidronate
Fosamax Plus D (Pro) /alendronate/cholecalciferol
Fosomax (Pro) /alendronate
Reclast (Pro) /zoledronic acid
Zometa (Pro)/zoledronic acid
Atelvia (Pro) /risedronate
Aclasta/zoledronic acid
Boniva (Pro) /ibandronate
Actonel (Pro) /risedronate
Actonel with Calcium (Pro) /calcium carbonate/risedronate
Aredia (Pro) /pamidronate
Binosto (Pro) /aldendronate
Skelid (Pro) /tiludronate
- Hildebolt CF (1997). Osteoporosis and oral bone loss. Dentomaxillofac Radiol 26:3-15.
- Eder A, Watzek G (1999). Treatment of a patient with severe osteoporosis and chronic polyarthritis with fixed implant-supported prosthesis: a case report. Int J Oral Maxillofac Implants 14:587- 590.
- von Wowern N, Klausen B, Kollerup G (1994). Osteoporosis: a risk factor in periodontal disease. J Periodontol 65:1134-1138
- Glaser DL, Kaplan FS. Osteoporosis. Definition and clinical presentation. Spine (Phila Pa 1976). 1997 Dec 15;22(24 Suppl):12S-16S. doi: 10.1097/00007632-199712151-00003. PMID: 9431639.
- Marx RE. Bone and bone graft healing. Oral Maxillofac Surg Clin North Am. 2007 Nov;19(4):455-66, v. doi: 10.1016/j.coms.2007.07.008. PMID: 18088897.
- Bouquot JE, McMahon RE. Neuropathic pain in maxillofacial osteonecrosis. J Oral Maxillofac Surg 2000; 58:1003-20.
- Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum 2002; 32:94-124.
- Gruppo R, Glueck CJ, McMahon RE, Bouquot J, Rabinovich BA, Becker A, et al. The pathophysiology of alveolar osteonecrosis of the jaw: anticardiolipin antibodies, thrombophilia, and hypofibrinolysis. J Lab Clan Med 1996;127:481-8.
- Damato K, Gralow J, Hoff A, Huryn J, Marx RE, Ruggiero S, et al. Available at: http://www.fda.gov/ohrms/dockets/ac/05/briefing/ 2005-4095B2_02_12-Novartis-Zometa-App-11.pdf. (Accessed Oct, 2008).
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003;61(9):1115–7.
- Woo SB, Hellstein JW, Kalmar JR. Bisphosphonates and osteonecrosis of the jaws. Ann Intern Med 2006; 144:753-6. [Erratum, Ann Intern Med 2006; 145:235.]
- Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment.
- Bilezikian JP. Osteonecrosis of the Jaw-Do Bisphosphonates pose a risk? N Engl J Med. 2006; 355:2278–81.
- Nelson B Watts, et al, Invasive Oral Procedures and Events in Postmenopausal Women With Osteoporosis Treated With Denosumab for Up to 10 Years, The Journal of Clinical Endocrinology & Metabolism, Volume 104, Issue 6, June 2019, Pages 2443–2452
- AAOMS Position Paper on Bisphosphonate-Related Osteonecrosis of the Jaws. Available at: http://aaoms.org/docs/position_papers/osteonecrosis.pdf. (Accessed October, 2008).


